The first three months of being a parent can be some of the most challenging. So much changes as you get to know this demanding, adorable little stranger, while trying to look after yourself as well. It’s all a learning curve, so go easy on yourself, and take help if it’s offered.
Remember, not only do you have to learn how to breastfeed, but your baby also needs to learn the best way to feed from the breast. And even if you’ve already breastfed one child, the next one can be different. But don’t stress – you’ll figure it out together.
Plunket is always here to help too. We’re here to help you if you’re having trouble with breastfeeding, or anything else. We have a lactation consultant service, or you can call PlunketLine any time – day or night - on 0800 933 922.
Here are some of the problems you may encounter while breastfeeding, and what you can do to deal with some of those issues.
Baby won’t breastfeed
It can be really upsetting if your baby suddenly refuses to breastfeed after they’ve been feeding well. Normally breastfeeding strikes only last a few days, but they can last as long as 10 days. And it can hurt (mentally as well as physically), or even make you feel pēpi doesn’t like you.
It's perfectly normal to feel that way, but rest assured your baby hasn't gone off you, just off the idea of feeding for some reason. Tell your midwife, Plunket nurse, or healthcare professional how you're feeling. They'll support you through this stage.
Try not to worry about it too much. It's just your baby's way of telling you that something's not right. There are any number of reasons why they may not be feeding. Perhaps:
- your baby has a cold
- your baby is uncomfortable or in pain
- your baby is having trouble attaching to your breast
- your baby is overtired, distracted, or overstimulated, which is normal in older babies
- your milk tastes different - it could be something you ate, medication you're taking, or hormonal changes (maybe you're about to have a period)
- your milk flow is slower to let down, or the flow is faster than usual
- your baby might prefer one breast over the other.
Most of these reasons are temporary, and will go away on their own; otherwise they can be sorted out with a few simple changes to your routine.
You could try:
- to relax and be as patient as you can
- a new feeding position
- hand-expressing some milk into your baby’s mouth, this might encourage them to feed
- giving your baby a breastfeed after their bath, when they’re warm and relaxed
- breastfeeding in a quiet place
- playing some relaxing background music, or feeding in a rocking chair
- offering a feed when your baby is first stirring from sleep or just going to sleep, or when baby is calm. You can use skin-to-skin contact to calm them, and you or your partner can do this.
- trying again later when your baby's more settled.
Baby biting breast
Some babies might like to bite once they’ve finished feeding, or to get your attention. Others may bite because they can’t wait to eat and the milk isn’t flowing fast enough. Whatever the reason, it can really hurt if baby bites you while you’re breastfeeding. Pulling them off the breast while they’re biting can be even more painful.
- Babies often bite at the very end of the feed. You could try to take them off when you sense they are coming to the end of the feed.
- Babies learn empathy very early on, so show your baby the bite has hurt you by giving a sad or painful expression.
- Avoid biting games with your baby; it is very tempting to say "you're so yummy" and mimic biting their little puku, but they may copy this behaviour at the worst times and use their real little teeth - ouch!
- If your baby’s a chomper, say ‘no’ calmly and firmly. Babies will usually release their bite when they hear you express pain and move. If they don't immediately release, you can gently put your little finger into the corner of their mouth to prompt them to stop biting.
- Try taking them gently off the breast when they bite by inserting your finger gently between the baby’s mouth and your nipple, have a short break, and then try again. Doing this every time they bite will teach them breastfeeding stops when they bite.
- You might also want to try offering your baby something else to chew on, like a teething ring.
- If the bite breaks the skin on your nipple it can lead to infection, so take care.
Sore and cracked nipples
Nipples shouldn’t be sore during the feed.
Possible causes are:
- the baby being in the wrong position at the breast
- using too high a setting on a breast pump
- wearing a nursing bra that’s too tight
- dry skin or skin conditions like eczema
- a thrush infection of the nipple, areola (the darker area around the nipple) and/or breast. Signs you may see and/or feel are:
- burning nipple pain
- flaking skin on the nipple or areola
- shiny skin on the nipple or areola
- painful breasts without tender spots or sore lumps
- stabbing pains in the breasts behind the areola.
If your baby’s mouth is infected, they may have one or more of the following symptoms:
- white patches inside their cheeks or on their tongue or gums that may look like leftover milk. When wiped off they leave red sore areas which may bleed.
- an uncomfortable or painful mouth, making them fussy during and between feeds. They may slip on and off the breast and may make a clicking sound.
See your GP or your midwife if you think you may have thrush.
To help heal sore and cracked nipples
- Avoid soap or cleansers when washing your nipples.
- Express a few drops of breast milk, gently massage it on your nipples, and allow it to dry.
- Leave your nipples uncovered or loosely covered between feeds to help them heal.
- Make sure your nipples dry completely after feeding.
- Change your nursing pads often, if you use them. This helps keep bacteria at bay.
- Paracetamol is safe to take for pain when you’re breastfeeding. Take it as directed on the packet, and see your health professional if pain persists.
See your health provider if the pain continues. If you can’t improve your baby’s position on the breast, and your nipples aren’t healing or are still painful, get help from PlunketLine on 0800 933 922, your midwife or doctor, Plunket nurse, or the La Leche League.
La Leche League can also help if you're having trouble breastfeeding.
Low milk supply
The size of your breasts and how full they feel aren't signs of how much milk the breasts hold. Generally speaking, the more milk your baby takes, the more the breasts make.
If you're worried about your milk supply, check in with your Plunket nurse, lactation consultant, or your GP to assess whether you really do have a low supply - a few simple tweaks might help.
Taking care of yourself is a great way to help your milk supply. Try to:
- eat healthy, nutritious meals and snacks. Your body needs lots of protein and healthy carbohydrate to keep you going, and to make milk
- make sure you drink enough water. Keep a sipper bottle within reach
- give yourself some time out to relax and de-stress. Let someone you trust watch your baby while you rest, go for a walk, take a shower, or just breathe! And sleep when the baby sleeps if you can
- try expressing with a breast pump after your baby has finished feeding to stimulate your milk supply.
Talk to your doctor, pharmacist, or Plunket nurse before taking herbal supplements or other remedies to boost your milk supply.
Engorgement or breast fullness
Breast engorgement is a common problem in the early days and weeks of breastfeeding. Once your baby is born, your breasts are given a signal to start full milk production. Blood flows to your breasts, and your milk usually comes in one to four days after the birth. Breast engorgement is when your breasts get swollen, hot and painful to touch.
To relieve breast fullness and engorgement try to:
- feed frequently, making sure your baby is attached well to avoid sore, cracked nipples
- gently express milk to soften the areola (darker area around the nipple). If it’s swollen, the baby can’t get onto the breast easily
- use different feeding positions or trying to feed lying down
- have a warm shower before feeding
- apply cool face cloths (flannels) on the breasts between feeds
- wear a comfortable, non-restrictive, supportive bra
- take paracetamol as directed on the packet for pain (see your health professional if pain continues for more than a couple of days).
Read more about oversupply and engorgement
Congested (blocked) milk ducts
Milk ducts can get congested. This is sometimes referred to as 'blocked ducts', 'plugged ducts' or 'plugging'.
Milk ducts are very fine, like small veins rather than large pipes. Just like your bowel, milk ducts have an important balance of good and bad bacteria. When this balance becomes uneven the duct becomes congested and narrows (but doesn’t block off completely).
Milk ducts carry milk from the round, "milk-making" cells to the nipple. If they are congested milk will start to build up in these cells causing pain and inflammation. Your breast may become painful, engorged over the area, and might also look red.
Sometimes a small white milk blister will appear on your nipple. This is called a bleb.
What causes milk duct congestion?
Milk duct congestion can be caused by:
- Withholding breastfeeding
- Too much pumping (especially in the early days)
- An over-production of milk (over-supply)
How to relieve duct congestion
- Feed from the affected breast first, when baby is sucking vigorously, but don’t favour this breast for long periods or do lots of "extra" feeds on this side
- Avoid pumping and trying to "empty the breast". Instead, use gentle hand expression until the breast feels "softened".
- Apply an ice pack over the inflamed area for 10-minute intervals as often as required
- Take pain relief and anti-inflammatory medication as directed/tolerated
- Avoid massage. These ducts are very small and sit behind a thick layer of skin and fatty tissue. The area is already swollen and sore, so deep massage may make it even more inflamed. GENTLE reverse pressure/lymphatic massage may help.
- Lymphatic/reverse pressure massage: Start your fingers on either side of the nipple and gently massage (using about the same pressure you would use to pat a cat) towards your chest and under your arm. See the below graphic for more info.
- Do not attempt to squeeze or remove the head of a milk bleb.
See your GP if you can't clear the lump in a few days, or sooner if you develop a fever or feel unwell, as this is a sign of mastitis (see below).
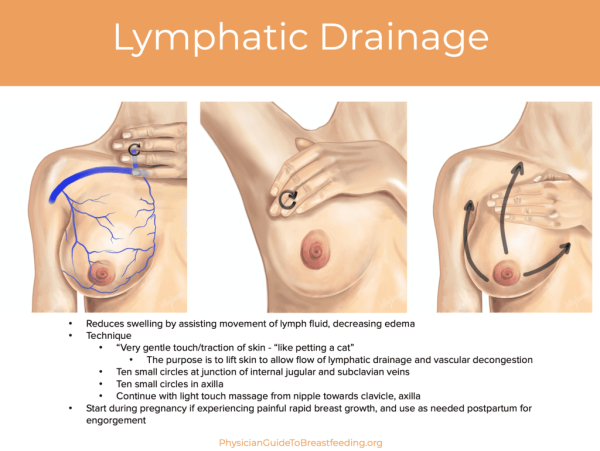
Lymphatic drainage diagram - PhysicianGuideToBreastfeeding.org
Mastitis (breast infection)
Mastitis is one name that covers a spectrum of breast infections. This includes:
- Inflammatory mastitis
- Bacterial mastitis
- Subacute mastitis
- Abscess
Inflammatory mastitis is not an infection and is usually the result of unresolved duct congestion. Some of the milk proteins can be forced into nearby breast tissue, and the tissue becomes inflamed. This is when the immune system is activated, and you get a systemic (full body) immune response. Antibiotics are not needed for inflammatory mastitis.
Bacterial mastitis is an infection and is usually caused by untreated inflammatory mastitis, or by bacteria entering the ducts from a nipple wound. Bacterial mastitis requires antibiotics. Some women who have no early signs of duct congestion still get mastitis.
Symptoms of inflammatory and bacterial mastitis can be very similar:
- aches and pains
- fever
- feeling shivery like the flu
- a painful pink or red and swollen area on the breast. The skin might be shiny and there may be red streaks.
If you have any of these symptoms, contact your midwife or doctor, or phone PlunketLine 24/7 on 0800 933 922 as soon as possible to speak to a nurse. You may need antibiotics to clear the infection.
If you have mastitis
- GENTLE reverse pressure/lymphatic massage may help to reduce the swelling. Follow the guidelines for clearing congested milk ducts or 'blocked ducts' above. Take care to avoid deep massage as this can lead to further inflammation.
- Get as much rest as possible – we know it’s hard to do when you’re a parent. Stay in bed if you can, sleep when your baby sleeps if you can, or at least put your feet up as much as you can. If you do go to bed, take everything you need with you - all you need to change nappies, food and drinks - so you don't have to keep getting up. Have your baby near you in their own safe sleep space, lying on their back with their face clear. If you have other children, it may be better to rest in your living area.
- Drink extra fluids.
- Keep feeding your baby. It’ll help your symptoms clear more quickly if you feed from the affected breast as "normally" as possible. The milk is perfectly safe for your baby to drink.
- You could try applying cold/ice packs to help reduce inflammation and swelling. Apply ice pack for 10-minute intervals and then repeat again after 30 minutes as required. Protect skin by wrapping ice packs in several layers of paper towel or a thin flannel.
- Try and get your baby to do most of the work removing milk from the affected side. But be mindful that feeding too much off the affected side can lead to engorgement and inflammation on the other side, or perpetuate a cycle of over-production in the affected breast.
- Try changing feeding positions to help drain multiple sections of the breast.
- If your baby won’t suck or fusses at the breast, it could be because mastitis can make your milk taste a bit salty. It can also be because the congestion is making the milk flow slower. If this is the case, you could hand-express the milk, or offer this side to the baby as the second side, or when they are a bit more relaxed and sleepy.
Make sure you visit your GP if you suspect you have mastitis, because you might need antibiotics. If antibiotics are prescribed, make sure you finish the whole course. Some mothers may get thrush after a course of antibiotics, so if you've had a thrush infection in the past, discuss this with your doctor.
If mastitis isn’t treated quickly, a breast abscess can form, which requires further treatment.
Mastitis and sore breasts
Babies with tongue-tie
Tongue-tie is something a baby is born with. In most pēpi, the piece of tissue under a baby’s tongue separates from the front end of the tongue before they’re born. Tongue-tie is when that piece of tissue is still attached to the front end of the tongue at birth.
A baby with tongue-tie might not be able to move their tongue freely.
If the tip of your baby's tongue looks heart-shaped when their tongue sticks out, can't reach the roof of their mouth or further than the edge of their lower lip, or can't move sideways, your baby may have a tongue-tie.
If you're breastfeeding and pēpi has tongue-tie, they might:
- have trouble latching or staying latched to your breast
- make a clicking sound when they're feeding.
- Your nipples might look squashed after feeding, and might feel sore or damaged.
Tongue-tie usually doesn’t need treatment, because the piece of tissue loosens itself as most babies get older. But sometimes that doesn't happen, and it might affect breastfeeding. If this is the case, your child can have a procedure called a frenectomy, which involves cutting the fold of tissue with a laser or scissors.
Talk to your health professional if you’re concerned. They can help you decide whether your pēpi needs a frenectomy, and which approach is best for your child.
